Root Canal Treatment in Ontario, CA: Compassionate Care, Costs, and Essential Insights

Root canal treatment is a precise endodontic procedure designed to eliminate infected dental pulp, disinfect the root canal system, and seal the tooth, providing relief from pain while preserving your natural ability to chew. In this article, we’ll walk you through how root canals function, the common signs that suggest you may need treatment, a detailed step-by-step overview of the procedure, realistic cost expectations for Ontario, CA, and helpful recovery tips to empower your decision-making. At Beautiful Smiles Ontario, we are dedicated to restoring your oral health and confidence through expert endodontic care, utilizing advanced technology and a patient-centered approach. We’ll discuss what to anticipate during diagnosis and treatment, when extraction might be a better option, post-operative care and pain management, as well as local cost factors—plus insights into how experienced clinicians like Dr. Hosny handle these cases to optimize long-term results. Keep reading to discover how to identify an infected tooth, what occurs during treatment, how pricing varies based on tooth type and complexity, and which option—root canal or extraction—best suits different clinical situations.
Ready to Experience Your Dream Smile?
Take the first step towards a confident, radiant smile. Our expert team is ready to provide a personalized assessment and discuss your unique goals.
How Can You Tell If You Need a Root Canal?
A root canal is typically necessary when the dental pulp becomes inflamed or infected, leading to persistent symptoms that indicate nerve involvement or a developing abscess. Early recognition of these signs is crucial to prevent the spread of infection and to preserve the tooth whenever possible. Common indicators include prolonged sensitivity to hot or cold, spontaneous or throbbing toothaches, swelling in the gums or face, and darkening of the tooth crown; these symptoms often require prompt evaluation. If you notice any of these signs, seeking immediate dental assessment can help minimize complications and expedite relief through appropriate endodontic therapy.

Identifying Tooth Pain and Sensitivity as Symptoms of a Root Canal
Tooth pain resulting from pulpitis often manifests as a deep, aching, or throbbing sensation that lingers even after the stimulus is removed, setting it apart from fleeting sensitivity. Persistent pain in response to hot or cold that lasts for minutes to hours typically indicates nerve inflammation or infection within the tooth rather than mere enamel sensitivity. Pain that disrupts your sleep, makes it hard to concentrate, or radiates to the jaw or ear suggests more advanced involvement and should prompt swift evaluation. If your pain patterns suggest an infected pulp, diagnostic imaging and clinical testing will follow to confirm the necessity for root canal therapy.
What Other Symptoms Suggest an Infected Tooth or Abscess?
In addition to pain and sensitivity, visible and systemic signs often accompany a tooth infection and may necessitate urgent care. Localized gum swelling, a sinus tract or “pimple” on the gum that drains pus, a persistent bad taste or odor, and facial swelling are common indicators of a periapical abscess. Fever, malaise, or spreading redness may signal a more serious infection that requires immediate attention from a dental professional. If you observe swelling, drainage, or systemic symptoms, reach out to a dentist promptly to mitigate the risk of complications and arrange timely intervention.
The most common red-flag symptoms for an infected tooth include:
Persistent, deep tooth pain that lingers after exposure to hot or cold. Swelling of the gums or face or the presence of a gum “pimple” with drainage. Discoloration of the tooth accompanied by ongoing sensitivity.
These symptoms collectively signal the need for diagnostic imaging and clinical testing to determine if endodontic therapy is necessary. Early detection enhances the likelihood of saving the natural tooth and avoiding more invasive alternatives.

What to Expect During a Root Canal Procedure: A Step-by-Step Guide
A root canal procedure methodically removes infected pulp, disinfects the root canal system, and restores the tooth to full function while preventing re-infection. The process begins with diagnostic imaging to map the canal anatomy, followed by anesthesia to ensure your comfort, then access and careful removal of infected tissue before cleaning, shaping, and sealing the canals. Modern endodontic care emphasizes precise instrumentation, effective irrigation protocols, and restorative planning so that the treated tooth can receive a definitive crown or onlay for lasting strength. Understanding each phase helps alleviate anxiety and clarifies why follow-up restoration is vital to protect the treated tooth.
The root canal workflow can be summarized with a focus on your experience and timing:
Diagnosis & Imaging: X-rays or CBCT assess canal anatomy and the extent of infection; this step defines treatment complexity and guides planning.
Anesthesia & Isolation: Local anesthesia and rubber dam placement ensure comfort and a dry field; most patients feel no pain during treatment.
Access & Pulp Removal: A small opening allows for the removal of infected pulp tissue using specialized instruments; debris is flushed with antimicrobial irrigants.
Cleaning & Shaping: Canals are shaped to receive a sealant; this process reduces bacterial load and prepares canals for filling.
Filling & Sealing: Canals are filled with biocompatible material and sealed to prevent reinfection; a temporary or permanent restoration is placed.
Final Restoration: A crown or onlay restores structural integrity and prevents fracture of the treated tooth.
This numbered sequence clarifies expectations and naturally leads into more detail about anesthesia and why crowns are commonly recommended after treatment.
What Happens During Root Canal Treatment: Anesthesia and Pulp Removal
Local anesthesia is administered to numb the tooth and surrounding tissues, ensuring you are comfortable throughout the procedure. Additional sedation options can be discussed for those who may feel anxious. Once numb, the clinician isolates the tooth with a rubber dam and creates a small access opening to reach the pulp chamber and root canal system. Using specialized instruments and irrigation solutions, the infected pulp is removed, and canals are shaped to allow effective disinfection; patients typically feel pressure or vibration but not sharp pain. Typical single-visit treatment times vary by tooth complexity; molar canals may require longer appointments or staged therapy in more complex cases.
Why Is a Dental Crown Often Necessary After a Root Canal?
A tooth that has undergone root canal therapy often becomes more brittle due to the removal of internal structures, increasing the risk of fracture without adequate protection. A crown or full-coverage restoration acts as a protective cap, restoring the tooth's shape and function while preventing cracks or re-infection at the margins. Temporary restorations safeguard the tooth between appointments, but a definitive crown provides long-term strength and an effective seal against leakage. Planning for timely restoration is a crucial part of endodontic success, ensuring that the disease-free tooth remains functional for years to come.
What Is the Cost of a Root Canal in Ontario, CA?
The cost of a root canal in Ontario, CA varies based on tooth type, treatment complexity, and whether specialist endodontic care or advanced imaging is necessary, resulting in a range rather than a fixed price. Anterior teeth generally cost less than premolars and molars due to their simpler anatomy and typically having a single canal, while multi-root molars require more time, instrumentation, and sometimes a referral to a specialist. Additional factors such as retreatment, post/core buildup, the need for CBCT imaging, and final crown placement can influence overall treatment costs. For an accurate estimate tailored to your tooth and insurance benefits, consult with your local provider to verify coverage and discuss payment options.
Factors that commonly influence root canal pricing:
Tooth anatomy and number of canals. Need for retreatment or prior failed endodontic therapy. Use of advanced imaging (CBCT), specialist fees, and restoration costs.
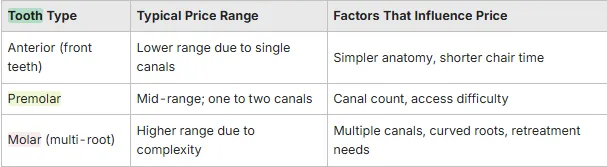
What Factors Affect Root Canal Pricing?
Several technical and logistical elements can change the complexity and, consequently, the cost of endodontic care, including tooth location, canal morphology, and previous root canal attempts. Cases requiring retreatment, removal of posts, or treatment of calcified or curved canals take longer and involve specialized tools, which can increase the fee. The use of three-dimensional CBCT imaging, referral to an endodontist versus treatment by a general dentist, and the need for a post and core or immediate provisional restoration can also add to overall costs. Understanding these variables helps patients set realistic expectations and evaluate long-term value compared to extraction and replacement options.
What Payment Options and Insurance Plans Are Available?
Insurance coverage for root canal therapy often depends on the specifics of your plan—many dental PPOs cover a portion of endodontic procedures, while others categorize restorative portions differently—so verifying your benefits is an important early step. Clinics typically assist patients by checking benefits before treatment, outlining what portion the insurer will cover and what the patient responsibility may be, and may offer payment plans or third-party financing to help manage costs. Discussing these options during your consultation helps align treatment planning with financial considerations and reduces unexpected surprises. Scheduling an evaluation allows the practice to provide a tailored estimate and explain available payment solutions.
Ready for Your Confident, Transformed Smile?
Take the definitive step towards achieving the radiant smile you deserve. Our expert team is prepared to provide a comprehensive, personalized evaluation and discuss your unique aesthetic and functional goals.
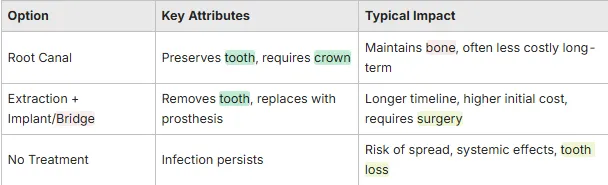
Root Canal vs. Tooth Extraction: Which Option Is Right for You?
Deciding between saving a natural tooth with a root canal or opting for extraction and replacement with an implant or bridge depends on factors such as restorability, infection control, patient health, timeline, and long-term cost implications. Root canal therapy preserves the tooth root and supporting bone, maintains natural occlusion and sensation, and often represents a conservative, cost-effective solution when the tooth is restorable. Extraction may be recommended when a tooth is non-restorable due to extensive fracture, severe bone loss, or when repeated endodontic failure leaves a poor prognosis. A comparative approach clarifies the pros and cons and supports patient-centered decisions.
What Are the Advantages of Saving Your Natural Tooth with a Root Canal?
Preserving your natural tooth maintains the root and surrounding bone, supports normal biting forces and tooth proprioception, and typically provides long-term function with appropriate restoration. Teeth that have undergone root canal treatment and received crowns often last many years, avoiding the surgical and prosthetic steps required for implants or bridges, which can increase costs and treatment time. Keeping your natural dentition also simplifies maintenance and reduces the need for alterations to adjacent teeth compared to bridge placement. When the prognosis is favorable, root canal therapy is a biologically conservative choice with high success rates.
When Is Tooth Extraction the Recommended Option Instead of a Root Canal?
Extraction is recommended when the tooth is structurally non-restorable due to severe fracture below the gumline, when root anatomy or resorption prevents adequate cleaning/sealing, or when repeated endodontic failures and persistent infection compromise prognosis. Patient medical conditions that contraindicate prolonged procedures or surgical considerations, as well as a patient preference for removal, also guide decisions toward extraction. After extraction, replacement options such as implants or bridges are discussed to restore function and aesthetics; however, these replacements involve additional procedures, costs, and healing time.
Decision criteria that often justify extraction:
Irreparable structural damage or insufficient remaining tooth to support restoration. Uncontrolled infection despite reasonable endodontic attempts. Medical or anatomic factors that make retreatment impractical.
What Can You Expect During Recovery from a Root Canal?
Recovery after root canal therapy typically involves a brief period of mild discomfort as surrounding tissues heal, with most patients returning to their normal activities within a few days. Effective pain management usually involves over-the-counter analgesics for 48–72 hours, while antibiotics are prescribed only when there is spreading infection or systemic involvement. Eating soft foods, avoiding heavy chewing on the treated tooth until a crown is placed, and maintaining gentle oral hygiene will support healing and reduce complications. Being aware of red-flag signs such as increasing swelling, persistent fever, or uncontrolled pain indicates the need to contact the treating office promptly.
How Long Does Recovery Take and What Are Common Aftercare Tips?
Initial post-operative discomfort usually peaks within the first 24–48 hours and then subsides; most patients report minimal pain after the first few days when managed with analgesics and rest. Full restoration of chewing function typically occurs after the permanent crown is placed, which is often scheduled several weeks after the root canal to allow for any necessary healing and final restorative planning. Aftercare tips include avoiding hard, crunchy foods on the treated tooth until finalized, practicing gentle flossing and brushing around the area, and attending follow-up visits to monitor healing. If swelling, fever, or persistent drainage develops, contact the practice for prompt reassessment.
Is Root Canal Treatment Painful? Addressing Patient Concerns
Modern root canal techniques, effective local anesthesia, and isolation strategies make the procedure comfortable for most patients, with many reporting that treatment is no more unpleasant than a routine filling. Pre-treatment anxiety can be managed through clear communication, topical anesthetics, and discussion of sedation options when appropriate; clinicians prioritize a calm, safe experience. Most of the pain associated with infected teeth occurs before treatment, and resolving the infection typically brings rapid relief. Understanding the steps, expected sensations, and available comfort measures helps reduce fear and improves adherence to recommended care.
Key points on pain and comfort: Anesthesia eliminates procedure pain; sensations are pressure and vibration rather than sharp pain. Post-operative discomfort is usually short-lived and manageable with common analgesics. Communication about anxiety and sedation options enhances patient experience and safety.

Why Choose Beautiful Smiles Ontario and Dr. Hosny for Your Root Canal?
Beautiful Smiles Ontario is committed to providing compassionate, high-quality dental care with advanced technology and prompt access for urgent needs—an approach that aligns with our mission to restore oral health and confidence for our local patients. Dr. Hosny is recognized as an expert in root canal treatment, and our practice highlights a warm, welcoming environment along with same-day services that help patients manage acute dental pain quickly. Those seeking endodontic care can expect clinician-level expertise combined with modern imaging and restorative planning to support durable outcomes. Our accolades and recognitions in local listings further reinforce trust signals for prospective patients evaluating their care options.
What Makes Dr. Hosny an Expert in Root Canal Treatment?
Dr. Hosny is recognized as an expert in root canal treatment, reflecting focused experience and a clinical emphasis on endodontic therapy within the broader scope of comprehensive dentistry. Our practice has a proven track record of serving the Ontario community and surrounding areas, and local recognitions cited in public listings underscore our commitment to clinical excellence. This background, combined with a patient-centered approach, supports predictable outcomes through careful diagnosis, use of contemporary techniques, and coordination of restorative follow-up. Patients benefit from clinician expertise when complex anatomy or retreatment issues arise.
How Does Beautiful Smiles Ontario Deliver Compassionate and Advanced Care?
Beautiful Smiles Ontario frames its care around a warm, welcoming environment, utilizing advanced technology to enhance diagnostic accuracy and treatment comfort, along with same-day services to address urgent dental pain swiftly. These elements combine to create a smoother clinical journey: advanced imaging clarifies anatomy before treatment, same-day access minimizes discomfort, and a compassionate team supports patient needs throughout recovery. For those seeking endodontic care that prioritizes both technical quality and patient comfort, our practice positions itself as a local resource for restoring oral health and confidence.
Reasons patients choose this approach:
Integration of modern diagnostic tools and treatment protocols for improved outcomes. Rapid access to care for urgent dental pain to limit the spread of infection. Patient-focused communication and restorative planning that preserves long-term function.
Frequently Asked Questions About root canals ?
1. What can I expect during the recovery period after a root canal?
Recovery after a root canal typically involves mild discomfort for a few days as the surrounding tissues heal. Most patients can return to their normal activities within 48 to 72 hours. Over-the-counter pain relievers are usually sufficient to manage any discomfort. It's important to avoid hard foods and maintain gentle oral hygiene around the treated area. If you experience increasing pain, swelling, or fever, contact your dentist promptly, as these may indicate complications that need attention.
2. How does a root canal compare to other dental procedures?
A root canal is often compared to tooth extraction, as both address dental issues caused by infection or damage. However, a root canal aims to save the natural tooth, preserving its root and surrounding bone, while extraction removes the tooth entirely. This can lead to further complications, such as bone loss. Root canals generally have a higher success rate and are less invasive than extraction followed by implant placement, making them a preferred option when feasible.
3. What are the long-term benefits of choosing a root canal?
Choosing a root canal can provide several long-term benefits, including the preservation of your natural tooth, which helps maintain jawbone density and alignment. A successfully treated tooth can last many years, often with proper restoration like a crown. This option is typically more cost-effective over time compared to extraction and replacement with implants or bridges, which involve additional procedures and costs. Overall, root canals support better oral health and function in the long run.
4. Are there any dietary restrictions after a root canal?
After a root canal, it's advisable to stick to a soft diet for the first few days to avoid putting pressure on the treated tooth. Foods like yogurt, mashed potatoes, and smoothies are good options. Avoid hard, crunchy, or sticky foods until your dentist places a permanent crown, as these can cause discomfort or damage to the tooth. Following your dentist's dietary recommendations will help ensure a smooth recovery and protect the treated area.
5. What should I do if I have anxiety about the procedure?
Feeling anxious about a root canal is common, but there are ways to manage this anxiety. Communicate your concerns with your dentist, who can explain the procedure in detail and discuss sedation options if needed. Many practices offer calming techniques, such as nitrous oxide or oral sedation, to help you feel more comfortable. Understanding the steps involved and knowing that modern techniques minimize discomfort can also alleviate fears and improve your overall experience.
6. How can I maintain my oral health after a root canal?
Maintaining oral health after a root canal involves regular dental check-ups, good oral hygiene practices, and a balanced diet. Brush twice a day and floss daily, especially around the treated tooth, to prevent plaque buildup. Avoid tobacco products, as they can hinder healing and increase the risk of complications. Following your dentist's aftercare instructions and attending follow-up appointments will help ensure the long-term success of your treatment and overall dental health.
What are the signs that a root canal may have failed?
Signs of a failed root canal can include persistent or worsening pain, swelling around the treated tooth, or the development of a new abscess. You may also notice a bad taste in your mouth or a foul odor. If you experience any of these symptoms, it's crucial to contact your dentist immediately for evaluation. Early intervention can help address complications and determine if further treatment, such as retreatment or extraction, is necessary.
Working Hours
Working Hours
Mon - Fri:
10 am - 6 pm
Sat-Sun:
Closed
Contact on
Contact on
Fax: (909) 984-4414
Address
Address
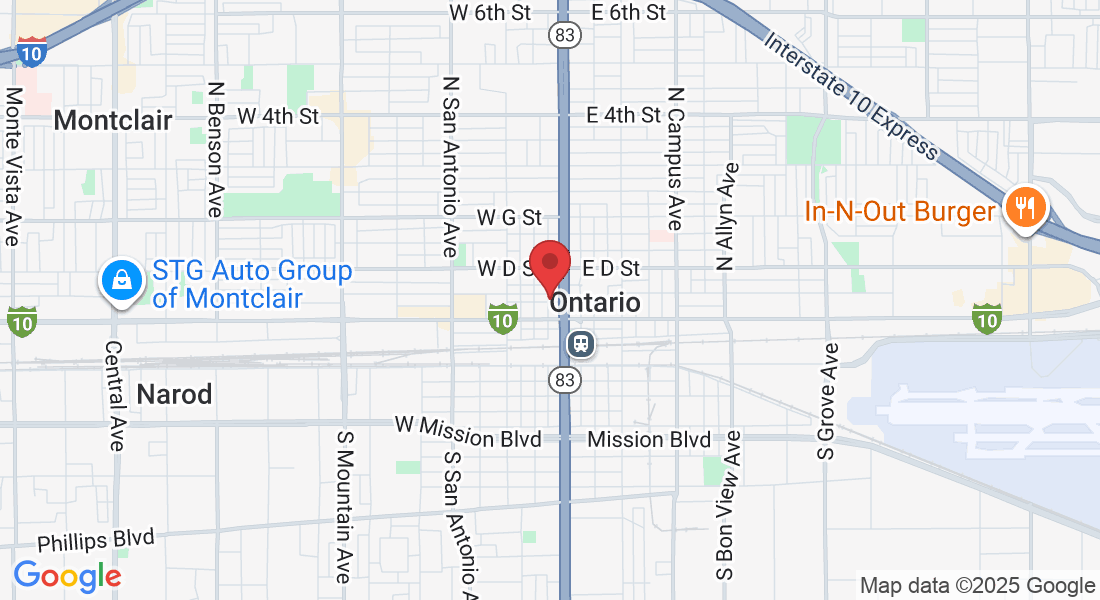
126 W B Street, Ontario, CA 91762, Ontario California 91762
Powered by Desert Marketing 2025. All Rights Reserved.