Gum Disease Treatment in Ontario, CA: Your Path to Healthier Gums

Gum disease, or periodontal disease, is a progressive infection that affects your gums and the supporting structures of your teeth. If left untreated, it can impact both your oral health and your confidence. In this article, we’ll explore what gum disease is, the differences between gingivitis and periodontitis, common causes and warning signs, and the evidence-based treatment options available right here in Ontario, CA. You’ll discover how non-surgical therapies like scaling and root planing work, when advanced procedures like gum grafting or bone grafting may be necessary, and how periodontal maintenance can help you keep your results. We’ll also discuss prevention strategies, the link between gum disease and systemic health issues like diabetes and heart disease, and what to expect in terms of timelines and costs. Finally, we’ll explain why choosing a practice that offers both oral surgery and implant services can simplify your restorative planning for more complex cases, and how to arrange a personalized consultation if needed.
Ready to Experience Your Dream Smile?
Take the first step towards a confident, radiant smile. Our expert team is ready to provide a personalized assessment and discuss your unique goals.
Understanding Gum Disease and Its Impact on Your Oral Health
Gum disease is an infection caused by bacterial plaque that leads to inflammation of the gums. If not addressed, it can progress to damage the periodontal ligament and the alveolar bone that supports your teeth. This process starts with the accumulation of biofilm on tooth surfaces; toxins from plaque trigger an immune response that, over time, results in pocket formation, tissue breakdown, and tooth mobility. Early-stage gum disease causes reversible inflammation, while advanced stages can lead to irreversible damage that affects chewing, aesthetics, and the ability to keep your natural teeth. Recognizing symptoms early and seeking targeted therapy can stop the progression and restore healthier oral conditions.

Gingivitis vs. Periodontitis: What’s the Difference?
Gingivitis is the initial, reversible stage of gum disease, marked by red, swollen gums that bleed easily when brushing or flossing. This inflammation is limited to soft tissue and does not involve bone loss; with proper plaque removal and improved oral hygiene, gingivitis can typically be resolved within days to weeks. Periodontitis occurs when inflammation extends deeper, forming periodontal pockets and causing loss of alveolar bone and attachment that cannot be fully reversed without surgical or regenerative therapy. Early identification of periodontitis allows for effective planning of scaling and root planing, and if necessary, regenerative procedures to stabilize your dental health and prepare for restorative options like implants.
Common Symptoms and Causes of Gum Disease
Gum disease often presents with symptoms such as bleeding during brushing, persistent bad breath (halitosis), swollen or receding gums, and in advanced cases, loose or shifting teeth and pus around the gums. Common causes include inadequate plaque control, tartar buildup, tobacco use, poorly managed systemic conditions like diabetes, certain medications that reduce saliva flow, genetic predisposition, and lifestyle factors such as diet and stress. These risk factors can increase harmful biofilm growth and intensify destructive immune responses, making prevention and targeted clinical management crucial for those at higher risk.
Watch for symptoms like bleeding gums, persistent bad breath, gum recession, and loose teeth.
Key causes include plaque buildup, tobacco use, systemic conditions (like diabetes), and medications affecting saliva.
Risk factors can accelerate disease progression and should inform personalized prevention and treatment plans.
Gingivitis can be reversed with professional cleaning and improved home care, while periodontitis may require deeper cleaning and surgical interventions to restore a stable oral environment.
Available Gum Disease Treatment Options in Ontario, CA
Gum disease treatment options range from non-surgical plaque control to advanced surgical and regenerative procedures, including restorative planning for teeth that cannot be saved. Initial therapy focuses on scaling and root planing to eliminate subgingival deposits and encourage reattachment; adjunctive local or systemic antimicrobials may be utilized as needed. For tissue defects and recession, soft-tissue grafts can restore gum margins and aesthetics, while bone grafting and guided tissue regeneration address alveolar bone loss to support future restorative work like implants. Periodontal maintenance and coordinated care with oral surgery or implant specialists complete the long-term management for many patients.
The Role of Scaling and Root Planing in Gum Disease Treatment
Scaling and root planing (SRP) is a non-surgical procedure designed to remove plaque and tartar from below the gumline and smooth root surfaces to minimize bacterial recolonization and inflammation. This process disrupts the harmful biofilm and allows for tissue healing and reattachment, typically resulting in reduced pocket depths and less bleeding during probing when followed by improved oral hygiene. SRP is usually performed under local anesthesia for your comfort and is followed by a re-evaluation to determine the need for maintenance or further intervention. Successful SRP often leads to a periodontal maintenance program to sustain results and prevent recurrence.
Advanced Treatments: Gum Grafting and Bone Grafting
Gum grafting and bone grafting are surgical options aimed at correcting soft-tissue recession and alveolar bone loss that can affect both function and aesthetics. Soft-tissue grafts enhance the width and thickness of gum tissue over exposed roots, reducing sensitivity, improving appearance, and protecting against further recession. Bone grafting reconstructs lost alveolar bone using graft materials and regenerative membranes to restore support, often as a precursor to dental implant placement when teeth cannot be saved. Healing timelines vary by procedure, and the success of regeneration depends on careful case selection, precise surgical technique, and adherence to postoperative care.
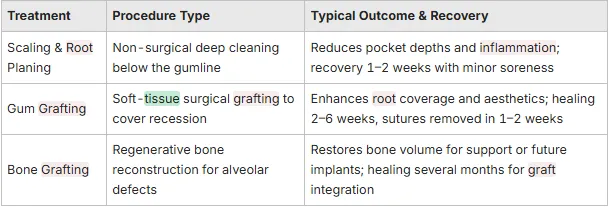
Different treatments yield distinct outcomes and recovery profiles; the table below compares common options to help patients quickly understand the differences.
The table outlines primary periodontal treatment options, expected outcomes, and typical recovery notes.
Preventing Gum Disease and Maintaining Healthy Gums
Prevention focuses on daily plaque control, modifying risk factors, and professional periodontal maintenance tailored to each patient’s unique needs. Effective home care includes brushing twice daily with proper technique, daily flossing or interdental cleaning, and using adjuncts like antiseptic mouth rinses when recommended. Lifestyle changes—such as quitting tobacco, managing blood sugar, maintaining a balanced diet, and reducing inflammatory triggers—support gum health. Regular professional care helps identify early changes, provides deep cleaning when necessary, and establishes a recall schedule to keep inflammation in check.
Understanding Periodontal Maintenance and Its Importance
Periodontal maintenance is a personalized program of professional cleanings and monitoring following active therapy to prevent recurrence and safeguard treatment outcomes. Maintenance visits typically involve subgingival instrumentation, monitoring pocket depths, and reinforcing home care techniques. Many patients benefit from three-month recall intervals after treatment for moderate to severe disease. Consistent maintenance has been shown to reduce tooth loss and protect your investment in treatment by controlling microbial load and promptly addressing any new disease activity. Long-term adherence to maintenance is a key factor in achieving stable periodontal health.
Oral Hygiene Practices to Prevent Gum Disease
Daily oral hygiene practices that help prevent gum disease include brushing twice daily with attention to technique, cleaning between teeth daily with floss or interdental brushes, and incorporating antimicrobial rinses when recommended by your clinician. Choosing the right tools and practicing gentle yet thorough brushing reduces plaque without harming soft tissue, while interdental cleaning targets the majority of plaque that accumulates between teeth. Patients with risk factors such as smoking or diabetes should collaborate closely with their dental team to modify behaviors and optimize systemic health, which directly impacts periodontal outcomes.
The following prevention checklist outlines practical steps you can adopt right away:
Brush twice daily using a soft-bristled brush and gentle circular strokes.
Clean between teeth daily with dental floss or interdental brushes suited to your spacing.
Schedule regular professional cleanings and adhere to recommended maintenance intervals.
Consistent daily care, combined with periodic professional support, creates a strong defense against gum disease progression and minimizes the need for invasive treatments.
The Connection Between Gum Disease and Overall Health
Emerging research highlights significant links between periodontal disease and systemic health conditions, suggesting that chronic oral inflammation can affect overall health through systemic inflammatory pathways and bacterial translocation. Periodontal pathogens and inflammatory mediators can enter the bloodstream, contributing to endothelial dysfunction and systemic inflammation associated with cardiovascular disease. Similarly, periodontal inflammation can complicate glycemic control in patients with diabetes, creating a bidirectional relationship where each condition exacerbates the other if not managed together. Recognizing these connections encourages collaboration between dental and medical providers to optimize patient outcomes.
The Impact of Gum Disease on Heart Health and Diabetes
Chronic periodontal inflammation adds to systemic inflammatory burden, potentially increasing risk factors for atherosclerosis and cardiovascular events through inflammatory mediators and bacterial components entering circulation. In diabetes, periodontal infection heightens systemic inflammation and insulin resistance, while effective periodontal treatment has been linked in some studies to improved glycemic control, illustrating a meaningful clinical connection. Current research supports that managing oral inflammation is a vital aspect of comprehensive care for patients with metabolic or cardiovascular concerns. Patients with chronic conditions should inform both their dental and medical teams to ensure coordinated care plans.
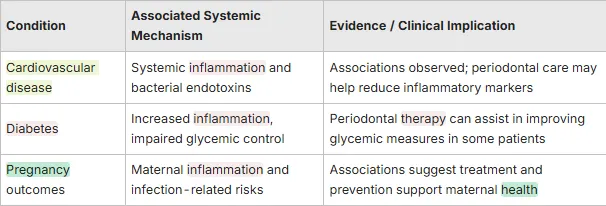
The table above summarizes key systemic links and plausible mechanisms.
Gum Disease and Pregnancy Outcomes
Research suggests a potential link between periodontal disease in pregnant individuals and adverse pregnancy outcomes, such as preterm birth and low birth weight. The systemic inflammation and bacterial presence associated with gum disease may contribute to these risks. Therefore, maintaining excellent oral hygiene and seeking periodontal care during pregnancy is crucial for both maternal and fetal health, and dental professionals often collaborate with obstetricians to ensure comprehensive care.
Ready for Your Confident, Transformed Smile?
Take the definitive step towards achieving the radiant smile you deserve. Our expert team is prepared to provide a comprehensive, personalized evaluation and discuss your unique aesthetic and functional goals.
Why Choose Beautiful Smiles Ontario for Your Gum Disease Treatment?
Beautiful Smiles Ontario is your trusted dental clinic in the Ontario, CA area, offering comprehensive periodontal care integrated with oral surgery and implant services for patients needing restorative planning. Our practice provides gum disease treatment alongside root canal therapy, dental implants, and general dentistry, ensuring coordinated care pathways when periodontal therapy and restorative rehabilitation are necessary. Dr. Hosny, our principal dentist, leads our clinical efforts to restore your oral health and confidence through compassionate, high-quality care. Patients seeking a family-friendly practice can expect a seamless care pathway that moves from diagnosis to treatment and long-term maintenance all within one coordinated setting.

Dr. Hosny’s Expertise in Periodontal Care
Dr. Hosny is the lead clinician for our practice’s clinical services, specializing in integrated care that includes oral surgery and implant planning for patients with advanced periodontal needs. His expertise helps align periodontal treatment with subsequent restorative options, minimizing fragmentation of care for patients who may require grafting or implants after disease control. This integrated model supports smoother transitions between therapy phases and clearer communication regarding prognosis and timelines. Patients are encouraged to discuss specifics of Dr. Hosny’s experience and procedural approaches during their consultation.
Enhancing Patient Experience Through Our Family-Friendly Approach
At Beautiful Smiles Ontario, we prioritize a family-friendly, patient-centered environment that emphasizes compassionate communication, clear explanations of diagnoses and treatment options, and supportive follow-up care for anxious patients and families. Our practice has received recognition in local reviews and awards, which many patients find reassuring when selecting a provider for complex care. Comfort measures, personalized education, and planned recall systems help patients adhere to periodontal maintenance and protect long-term results. Scheduling a consultation allows our team to create a tailored plan that balances clinical needs with patient preferences and practical considerations.
Integrated services at one practice simplify coordination for complex rehabilitations.
Patient education and follow-up reinforce home care and maintenance adherence.
A family-oriented environment supports patients of all ages through preventive and restorative stages.
Understanding Gum Disease: Causes, Symptoms, and Risks
The costs and timelines for gum disease treatment can vary based on the severity of the disease, the number and type of procedures required, and any restorative needs that follow periodontal therapy. Non-surgical care like scaling and root planing is typically completed over one to a few visits, with follow-up re-evaluation, while surgical grafting and regenerative procedures require operative visits and a staged healing period before potential implant placement. Major cost factors include diagnostics, the extent of debridement or surgery, graft materials, and any implant or restorative components needed later. Exact costs depend on individual circumstances, so we encourage patients to schedule a consultation to receive a personalized estimate and discuss available insurance or financing options.
Duration of Gum Disease Treatment
Non-surgical treatment often requires one to three visits for full-mouth debridement, with an initial re-evaluation within four to twelve weeks to confirm healing and determine maintenance intervals. Surgical grafting procedures involve an operative visit followed by staged healing over weeks to months, during which soft tissue and bone integration are assessed before definitive restorative work. When implants are planned, additional healing and integration periods are necessary, making full rehabilitation a multi-month process in many cases. The variability in timelines underscores the importance of individualized treatment planning and close monitoring during recovery.
Typical Costs and Insurance Options
Cost components for periodontal care include diagnostic imaging and exams, scaling and root planing sessions, surgical fees for grafting, graft materials and membranes, and any later restorative or implant-related work. Many dental insurance plans cover portions of periodontal treatment, while other costs may be out-of-pocket; patients should review their benefits and discuss available financing or phased treatment options with our practice. Beautiful Smiles Ontario recommends scheduling a consultation to obtain an individualized estimate and to learn about our approach to working with insurance and payment plans where applicable.
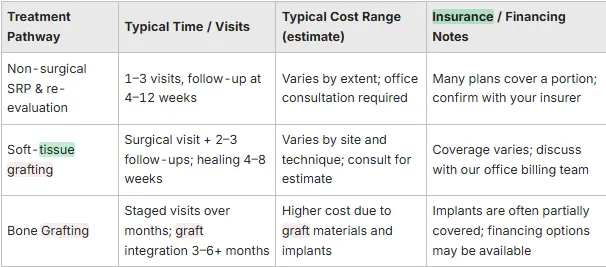
The following table outlines typical time and cost expectations for common periodontal pathways; exact figures require a consultation.
This table clarifies the major components that influence cost and timing while emphasizing the importance of personalized estimates. Contacting our practice to schedule an evaluation is the recommended next step for a tailored plan and accurate financial guidance.
Key cost drivers include severity, surgical needs, and restorative implants.
Insurance may cover portions of periodontal care; verify your benefits ahead of treatment.
A consultation provides an individualized timeline and estimate to guide your decisions.
Frequently Asked Questions
Untreated gum disease can lead to serious consequences, including tooth loss, bone deterioration, and an increased risk of systemic health issues. As the infection progresses, it can cause irreversible damage to the supporting structures of your teeth, leading to mobility and eventual loss. Additionally, chronic inflammation from gum disease has been linked to conditions such as heart disease and diabetes, making early intervention crucial for both your oral and overall health.
For effective gum disease prevention, it’s generally recommended to visit the dentist every six months for routine check-ups and cleanings. However, individuals with a history of gum disease or other risk factors may benefit from more frequent visits, such as every three to four months. Regular professional cleanings help remove plaque and tartar buildup, monitor gum health, and provide personalized advice on maintaining optimal oral hygiene.
Absolutely! Lifestyle changes can significantly impact the management and prevention of gum disease. Quitting smoking, maintaining a balanced diet rich in vitamins and minerals, and managing stress levels can enhance gum health. Additionally, controlling systemic conditions like diabetes through diet and medication can reduce the risk of periodontal complications. Adopting good oral hygiene practices, such as regular brushing and flossing, is also essential for effective gum disease management.
During a periodontal maintenance visit, your dentist will perform a thorough cleaning that includes scaling and root planing to remove plaque and tartar from below the gumline. They will also monitor pocket depths, assess gum health, and provide guidance on home care techniques. These visits are crucial for preventing the recurrence of gum disease and typically occur every three to six months, depending on your individual needs and treatment history.
While professional treatment is essential for managing gum disease, certain home remedies can complement your oral care routine. Rinsing with warm salt water can help reduce inflammation and promote healing. Additionally, using antimicrobial mouthwashes may help control bacteria. However, these remedies should not replace regular dental visits or professional cleanings, as they cannot effectively address the underlying causes of gum disease.
Signs that gum disease may be worsening include increased gum bleeding during brushing or flossing, persistent bad breath, gum recession, and loose or shifting teeth. If you notice any of these symptoms, it’s crucial to consult your dentist promptly. Early intervention can prevent further progression and help restore gum health through appropriate treatment options.
Nutrition plays a vital role in maintaining gum health. A diet rich in vitamins C and D, calcium, and antioxidants can support gum tissue and reduce inflammation. Foods like fruits, vegetables, whole grains, and lean proteins contribute to overall oral health. Conversely, a diet high in sugar and processed foods can promote plaque buildup and increase the risk of gum disease. Therefore, a balanced diet is essential for preventing and managing periodontal issues.
