
A Guide to Understanding Dental Implants
Understanding Dental Implants: A Guide for Ontario Residents

What Are Dental Implants in Ontario and How They Restore Your Smile
Dental implants in Ontario restore missing teeth by anchoring biocompatible fixtures directly into the jawbone, creating a foundation for natural-looking crowns that improve function and appearance. Whether you’re dealing with a single gap or a full-arch restoration, implants eliminate slipping dentures and prevent bone loss by replicating tooth roots. In this comprehensive guide for dental implants, you will discover:
The definition and anatomy of dental implants and their key components
The biological process of osseointegration that secures implants
Each step of the implant procedure from consultation to crown placement
The various implant types available in Ontario and how to choose the right option
Benefits, potential risks, candidacy criteria, maintenance tips, cost considerations, and how implants compare to bridges and dentures
Drawing on advanced technology and patient-centered care, Ontario’s implant specialists deliver long-term oral health solutions that restore confidence and chewing efficiency.
What Are Dental Implants and Their Key Components?
Dental implants replace missing teeth with artificial roots and crowns that mimic natural anatomy. Each implant system combines a fixture, connector, and prosthesis to support chewing, speech, and smile aesthetics.
Osseointegration locks the fixture in place, enabling the implant to withstand normal biting forces while preserving jawbone density. Understanding these parts lays the groundwork for exploring how implants fuse with bone and what to expect during treatment.
What Is a Dental Implant and How Does It Replace a Missing Tooth?
A dental implant is a medical device consisting of a metal or ceramic post surgically embedded in the jawbone to act as a substitute root. This fixture integrates with the surrounding bone through osseointegration, forming a stable anchor for an abutment and prosthetic crown. For example, a titanium post placed in the mandible can support a porcelain crown that restores chewing capacity and prevents adjacent teeth from shifting, ensuring both function and aesthetics.
What Are the Main Parts of a Dental Implant?
The three essential components of a dental implant system work together to replicate a full tooth structure.
Implant Post (Fixture):A screw-shaped rod inserted into bone to act as an artificial root.
Abutment (Connector):A small collar that joins the post to the crown.
Crown (Prosthesis):A custom-shaped tooth-colored cap that restores appearance and function.
Each component plays a critical role in transferring bite forces, securing the restoration, and providing a lifelike result that integrates seamlessly with surrounding tissues

What Materials Are Used in Dental Implants? Titanium vs. Zirconia Explained
Implant materials determine biocompatibility, strength, and aesthetics. Below is a comparison of the two most common options:
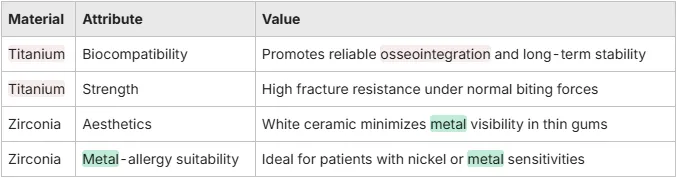
Both materials support predictable outcomes, but your Ontario implant specialist will recommend the best choice based on bone quality, gum thickness, and personal preferences.
How Do Dental Implants Work? Understanding the Osseointegration Process
Dental implants achieve stability through a biological bonding process called osseointegration, in which bone cells attach directly to the implant surface. This fusion creates a durable interface that withstands chewing forces and prevents the bone resorption that follows tooth loss.
Before exploring surgical steps, it’s essential to examine how the body interacts with implant materials to ensure long-term success.
What Is Osseointegration and Why Is It Crucial for Implant Success?
Osseointegration is the direct structural and functional connection between living bone and the surface of a load-bearing implant. By encouraging osteoblasts to deposit new bone around the fixture, this process secures the implant with natural bone density and prevents micromovement that can cause failure. Successful osseointegration underpins the implant’s ability to restore chewing efficiency and preserve jaw structure over decades.
Osseointegration and Implant Success
Osseointegration is the direct structural and functional connection between living bone and the surface of a load-bearing implant. This process is crucial for the long-term success of dental implants, as it ensures the implant integrates with the jawbone, providing stability and preventing bone loss.
Branemark, P. I., Osseointegration in Clinical Dentistry (1985)
This research is fundamental to understanding how dental implants work and why osseointegration is essential for their success.
How Does Titanium Encourage Osseointegration?
Titanium forms a titanium-oxide layer on its surface that attracts bone-forming cells, enabling robust fusion. This passive film resists corrosion and creates a biocompatible interface that osteoblasts readily colonize. As a result, titanium implants exhibit success rates above 95% when placed by experienced Ontario clinicians using guided surgical protocols.
Titanium and Osseointegration
Titanium is a commonly used material in dental implants because it forms a titanium-oxide layer on its surface, which attracts bone-forming cells. This biocompatible interface allows osteoblasts to colonize the implant, leading to robust fusion and high success rates.
Buser, D., et al., Titanium implants in bone (1991)
This research supports the article's explanation of how titanium promotes osseointegration, a key factor in the success of dental implants.
What Is the Typical Healing Timeline After Implant Placement?
-Initial Healing (0–2 weeks): Soft tissue closure around the surgical site
-Bone Fusion (2–12 weeks): Osseointegration where bone cells adhere to the fixture
-Restoration Phase (12+ weeks): Attachment of the abutment and crown
During this timeframe, patients experience progressive stability and can transition from temporary restorations to the final prosthesis, regaining full function and comfort.

Dental Implant Procedure and Healing Timeline
The dental implant procedure involves several well-defined stages, including initial consultation, surgical placement, healing, abutment attachment, and crown placement. The healing timeline typically spans 3–6 months, with different phases of healing occurring during this period.
Esposito, M., et al., Interventions for replacing missing teeth: dental implants in adults (2007)
This research provides a comprehensive overview of the dental implant procedure and the expected healing timeline, which aligns with the article's description of the process.
What Is the Step-by-Step Dental Implant Procedure?
Dental implant treatment unfolds through a series of well-defined stages that ensure precision and patient comfort. Below is an overview of each phase before delving into details.
1. Initial Consultation and Planning
2. Surgical Placement of Implant Post
3. Healing and Osseointegration Period
4. Abutment Attachment
5. Crown Placement and Final Restoration
These coordinated steps deliver reliable outcomes, supported by digital imaging and guided surgery techniques that Ontario implant specialists employ to optimize implant positioning and reduce complications.
What Happens During the Initial Consultation and Planning?
During consultation, the dentist evaluates overall health, reviews medical history, and conducts a comprehensive oral exam, including 3D imaging. This planning phase determines bone volume, nerve location, and ideal implant size and position. A tailored treatment plan, often using CAD/CAM technology, maps implant placement for predictable outcomes and streamlined surgery.
How Is the Implant Post Surgically Placed into the Jawbone?
Under local anesthesia or light sedation, the surgeon creates a small incision in the gum to expose the bone and drills a precise osteotomy. The implant post is then inserted and torqued to ensure primary stability. The incision is sutured for soft-tissue healing, and temporary restorations may be placed to maintain appearance during osseointegration.
What Are the Steps for Abutment and Crown Placement?
Once osseointegration is confirmed, the abutment is attached by exposing the implant and securing the connector piece. After soft tissues heal around the abutment, a custom crown is fabricated—either cement-retained or screw-retained—and affixed to complete the restoration. This final step restores full chewing function and integrates seamlessly with neighboring teeth.
How Is Post-Operative Care Managed for Optimal Healing?
After each surgical stage, patients follow a regimen of gentle brushing, antimicrobial rinses, and dietary modifications to support tissue health. Regular follow-up visits monitor healing, manage any discomfort with analgesics, and verify that osseointegration is progressing. Effective aftercare directly influences implant longevity and patient satisfaction.
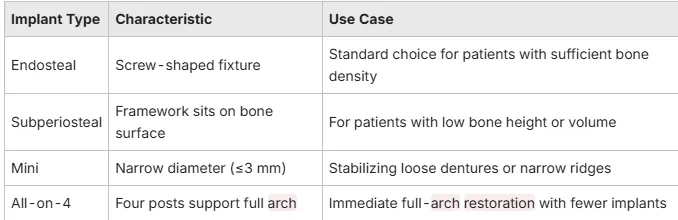
What Types of Dental Implants Are Available? Choosing the Best Option in Ontario
Ontario patients can select from several implant styles based on anatomy, restoration needs, and bone conditions. Each type offers unique advantages for different clinical scenarios. Understanding these options helps you and your Ontario dentist decide whether conventional endosteal implants, specialized subperiosteal frameworks, low-invasive mini implants, or All-on-4 protocols best suit your oral anatomy and restoration goals.
What Are the Benefits and Potential Risks of Dental Implants?
Dental implants offer lasting advantages but carry considerations that patients should weigh before treatment.
-Key benefits include:
-Enhanced chewing efficiency and speech clarity
-Preservation of jawbone volume and facial structure
-Natural aesthetics that boost confidence
-Longevity with success rates above 95%
Potential risks to discuss:
-Surgical infection or delayed healing
-Nerve irritation leading to temporary numbness
-Sinus complications in upper jaw placements
Implant dentistry’s safety and predictability increase when performed by experienced Ontario specialists who follow strict protocols and maintain rigorous sterilization standards.
Who Is a Good Candidate for Dental Implants in Ontario?
Ideal implant candidates enjoy good overall health, sufficient bone density, and healthy gum tissues.
Key eligibility criteria include:
-Absence of uncontrolled systemic conditions (e.g., diabetes)
-Adequate jawbone height and volume, possibly augmented by grafting
-Commitment to oral hygiene and regular dental check-ups
Your dentist will assess suitability through clinical exams and CBCT scans. Even patients with minor bone loss often qualify after preparatory procedures, broadening access to implant-based restorations.
How Should You Care for Dental Implants to Ensure Longevity?
Proper maintenance preserves implant health and function for decades.
Essential practices include:
-Brushing twice daily with a soft-bristle brush to remove plaque
-Flossing around the abutment interface to prevent biofilm buildup
-Using interdental brushes or water flossers to clean hard-to-reach areas
Regular professional visits every 3–6 months allow hygienists to assess implant stability, measure bone levels, and address early signs of inflammation before they progress. Vigilant aftercare supports implant success and prevents peri-implant disease.
How Do Dental Implants Compare to Other Tooth Replacement Options?
When evaluating implants, bridges, and dentures, consider function, bone health, and aesthetics:
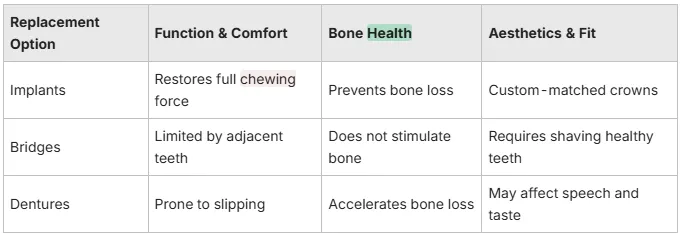
By preserving jawbone integrity and offering stable prosthetics, implants outperform conventional bridges and removable dentures in long-term oral health and daily comfort.
What Are the Typical Costs, Insurance, and Financing Options for Dental Implants in Ontario?
Dental implant expenses vary by complexity, materials, and preparatory procedures. Typical cost ranges in Ontario:
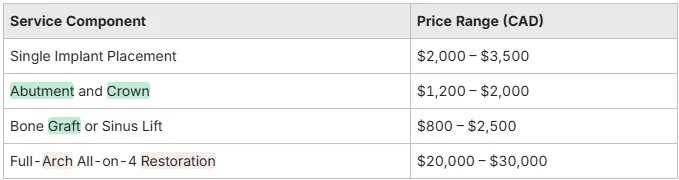
Many insurance plans cover a portion of implant surgery or crown fabrication. Dental offices often partner with third-party financiers to offer monthly payment plans, making implant treatment accessible through interest-free options or low-interest financing aligned with patient budgets.
In Ontario, dental implants deliver predictable, long-lasting tooth restoration by replicating natural root-to-crown anatomy. Advances in materials like titanium and zirconia, digital planning, and guided surgery have elevated success rates above 95 percent while minimizing recovery times. By understanding the components, osseointegration, procedural steps, and maintenance requirements, patients can make informed decisions about implant therapy. Consult with a qualified Dentist Ontario implant specialist to explore personalized treatment options and reclaim full oral function and confident smiles.
